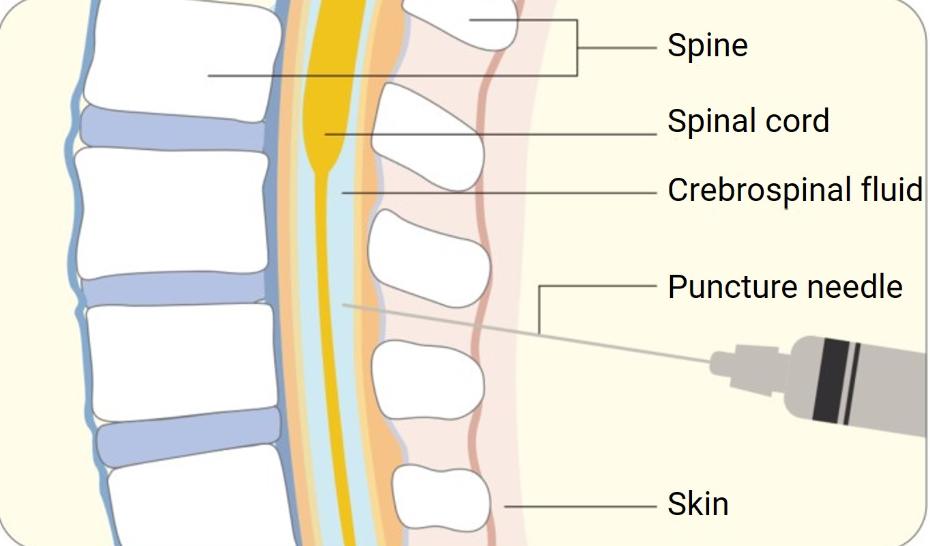
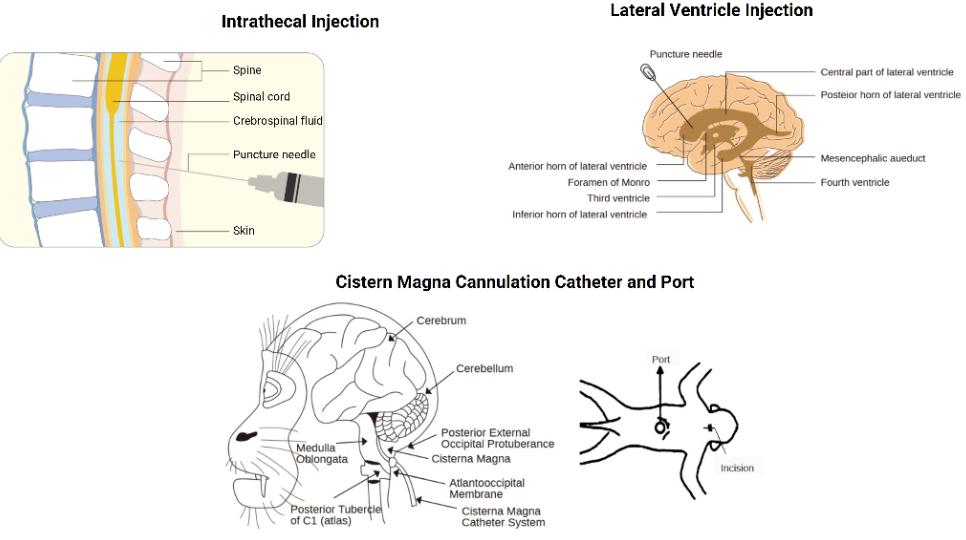
Central Nervous System (CNS) infections represent a critical challenge in medicine due to their complexity and potential severity. The blood-brain and blood-cerebrospinal fluid (CSF) barriers make delivering effective concentrations of antibiotics into the CNS difficult. Consequently, traditional intravenous (IV) therapies often fall short. Intrathecal therapy, which involves direct drug delivery into the CSF, offers an alternative that promises targeted treatment. By bypassing systemic limitations, intrathecal therapy could increase therapeutic success rates for CNS infections. This article examines the suitability of intrathecal therapy for such infections, discussing its advantages, potential risks, and best practices.
Why CNS Infections Demand Special Delivery
Blood–brain and Blood–CSF Barriers
These barriers are selective permeability layers, tightly regulating substances entering the brain. Comprised mainly of endothelial cells in the blood-brain barrier and epithelial cells in the blood-CSF barrier, they prevent systemic drugs from easily penetrating the CNS. For antibiotics to operate effectively, they must be both small and lipophilic, traits not all possess. The barriers’ selectivity often necessitates alternative delivery methods, such as intrathecal administration, to achieve therapeutic drug levels in the CNS, essential for managing infections like meningitis or encephalitis.
Limits of Systemic Antibiotics
Systemic antibiotics are the conventional response to bacterial infections. However, their efficacy diminishes when it comes to the CNS due to inadequate penetration capabilities. The limitations arise from the inability of many antibiotics to cross the CNS barriers in therapeutic concentrations. Furthermore, higher systemic doses required to achieve CNS penetration can result in toxicity. Intrathecal therapy circumvents these issues by enabling direct drug administration into the CSF, where it can exert the desired antimicrobial effects more efficiently.
When Intrathecal Therapy Makes Sense
Intrathecal therapy stands out when conventional methods fail, offering a strategic option for CNS infections resistant to standard treatments. Its targeted approach is especially relevant in challenging scenarios involving resistant pathogens or device-related infections.
Multi‑resistant Pathogens and Inadequate IV Therapy
The rise of multi-resistant pathogens poses significant challenges in treating CNS infections, as they can render IV antibiotics ineffective. Intrathecal therapy becomes crucial in these cases, ensuring that potent antibiotics bypass resistance mechanisms by targeting bacteria directly within the CNS. This method allows for high local concentration, enhancing antibiotic efficacy and offering hope in otherwise intractable infections.
Cases of Device‑related CNS Infections
Devices like shunts or drains can become breeding grounds for infections, complicating treatment due to biofilm formation. Intrathecal therapy can address these device-related infections by delivering antibiotics that penetrate and disrupt biofilms in the CNS. This focused approach enhances treatment outcomes and helps manage infections that are otherwise difficult to eradicate via systemic methods.
Clinical Evidence and Outcomes
Research and clinical trials provide insight into the efficacy and safety of intrathecal therapy for CNS infections. Understanding the existing evidence aids in informed decision-making for healthcare professionals.
Intraprofessional Reviews and Drug Classes
Intrathecal therapy involves a collaboration of neurologists, infectious disease specialists, and pharmacists to optimize drug regimens. Reviews of clinical practices highlight the use of various drug classes, such as aminoglycosides and glycopeptides, administered intrathecally. Such collaborations help tailor treatments to patient-specific needs, reflecting the multidisciplinary approach needed for successful outcomes.
Recent Clinical Studies
Recent studies underscore the effectiveness of intrathecal therapy in treating complex CNS infections. Outcomes indicate improved survival rates and reduced complications when compared to systemic treatments alone. By examining these studies, we gain an insight into how direct delivery can significantly enhance therapeutic impacts.
Safety, Risks, and Practical Issues
While promising, intrathecal therapy involves certain risks and demands careful consideration of procedural and practical factors.
Procedural Risks and Complications
Procedural risks such as infection, bleeding, or nerve damage accompany intrathecal administration. The most significant concerns include mechanical injury during catheter placement and potential dose-related neurotoxicity. Proper technique and monitoring are vital to minimize such risks and ensure patient safety during treatment.
Dosing, Monitoring, and Delivery Systems
Precision in dosing is crucial to avoid both subtherapeutic levels and toxicity. Advanced delivery systems, including programmable pumps, enable controlled and continuous drug delivery. Regular monitoring of drug levels in the CSF ensures sustained efficacy and safety, allowing clinicians to adjust dosages as needed for optimal patient outcomes.
Best Practices from Preclinical and Industry Insights
Preclinical research and industry expertise provide guidelines for the effective use of intrathecal therapy. Best practices involve incorporating pharmacokinetic modeling to predict optimal dosing strategies and leveraging technological advancements in delivery systems for precise control. Collaborative efforts between researchers and industry can refine these therapies, improving treatment protocols and patient outcomes.
Conclusion
Intrathecal therapy presents a viable alternative for challenging CNS infections, especially where systemic treatments fall short. By overcoming the natural barriers of the CNS, it offers targeted, efficient drug delivery, though not without risks. The decision to employ intrathecal therapy should consider patient-specific factors, infection severity, and potential complications. With ongoing research and refinement of techniques, intrathecal therapy holds promise for enhancing CNS infection management, offering new hope to patients and clinicians alike.